3 Challenges physicians face in providing care for their epilepsy patients
Epilepsy is a complicated condition for both patients living with the disease and the physicians that treat them. There are various types of seizures that can be caused by many factors, and it is difficult to diagnose the type even through an accurate description of an event [1]. Although it can still be hard for a patient to become seizure-free, there is a range of treatment options like anti-epileptic drugs and surgery, which can help control seizures.
This is why the ongoing monitoring of people living with epilepsy is so crucial, especially when it comes to making the right decisions to provide the best possible care and medication.
In this blog post, we’ll discuss 3 challenges that physicians may face when caring for their epilepsy patients and how our new Remote Seizure Monitoring service may be able to help. Let’s get started!
1. Was it really a seizure?
Since seizures are often identified based on what an observer has seen, it is extremely important to have objective data to understand if a patient actually had a seizure and to distinguish, if possible, what type of seizure they had. This information will guide treatment decisions that doctors will make.
According to the Epilepsy Foundation, there are now 3 new classifications of seizure types that were developed to name seizures in a more accurate, less confusing, and more descriptive way. There are generalized onset seizures, focal onset seizures, and unknown onset seizures. Each seizure classification separates the symptoms into groups that involve movement [2].
However, it can be difficult for a physician to determine whether a patient actually had a seizure and to also understand what kind of seizures they have. For physicians, witness testimony that can give an accurate description of events can be very helpful to determine if a seizure actually occurred [1]. However, the education level of an observer influences how accurately they may describe and classify events as epileptic and non-epileptic [3-4], which means that sometimes events may be falsely interpreted as seizures, and the seizure types themselves may not be correctly identified.
2. Video EEGs: a gold standard but far from perfect
For epilepsy specialists, prolonged EEG-video is considered the gold standard for evaluating if a person is having seizures. This can be performed in both inpatient and ambulatory settings, yet each has their advantages and disadvantages [5].
For instance, in the hospital, medications can be safely reduced to try to induce a seizure. One of the biggest challenges behind this is that it may be impossible for a patient to take time off work and stay in the hospital for a few days. Instead, in the ambulatory setting, the seizure may not be caught on camera or results may be inconclusive and require an eventual inpatient session [5].
EEGs are costly, and their cost increases with the amount of monitoring time. In one analysis, “to identify one child with seizures using 1 hour of EEG monitoring costs $466, to identify one more child with 24 hours of monitoring costs $1666, and to identify one additional child with 48 hours of monitoring costs $22,648” [6].
Though an initial EEG examination is crucial in diagnosing a patient with epilepsy, up until now, there is still no perfect, ideal solution to monitor someone’s seizure activity outside the clinic for a prolonged period of time.
3. Patients don’t record all of their seizures
Though paper diaries are still the most common method of recording seizures, when using them, patients misreport about 56% of all seizures they’ve had. This increases to about 86% for nocturnal seizures. Inaccuracy can also be attributed to postictal seizure unawareness, so patient seizure counts are not reliable sources for seizure information [7], making it harder for doctors to have dependable information upon which to provide data-driven care.
Overcoming challenges in seizure monitoring
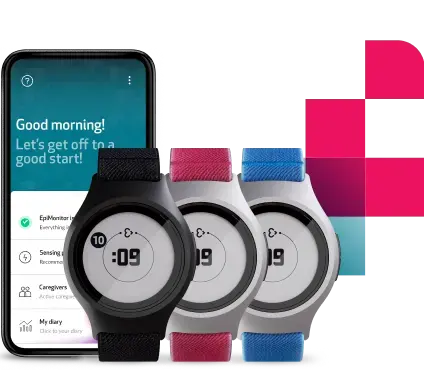
Challenges like the above sometimes present real obstacles in enabling physicians to provide their patients with the best possible care. That is why we have taken the FDA-cleared technology of Embrace2 and developed a new solution for physicians, Remote Seizure Monitoring.
Discover more about our new Remote Seizure Monitoring service that aims to empower physicians to make data-driven decisions for their epilepsy patients on our website, or fill out this quick form to get contacted by a member of our team.
Words worth reading
Sources:
1. https://www.epilepsy.com/learn/diagnosing-epilepsy
2. https://www.epilepsy.com/learn/types-seizures
3. Ristić AJ, Drašković M, Bukumirić Z, Sokić D. Reliability of the witness descriptions of epileptic seizures and psychogenic non-epileptic attacks: a comparative analysis. Neurol Res. 2015;37(6):560–562.
4. Brophy, G., Sarma, A., Khandker, N., & Kurczewski, L. (2016). Medical management of epileptic seizures: challenges and solutions. Neuropsychiatric Disease And Treatment, 467. doi: 10.2147/ndt.s80586
5. https://www.epilepsy.com/learn/diagnosis/eeg/which-eeg-type-best-you
6. Abend NS, Topjian AA, Williams S. How much does it cost to identify a critically ill child experiencing electrographic seizures?. J Clin Neurophysiol. 2015;32(3):257–264. doi:10.1097/WNP.0000000000000170
7. Hoppe C, Poepel A, Elger CE. Epilepsy: Accuracy of Patient Seizure Counts. Arch Neurol. 2007;64(11):1595–1599. doi: https://doi.org/10.1001/archneur.64.11.1595