Am I having seizures while sleeping?
One of the main concerns of living with epilepsy is making sure that you get help fast during a seizure. In the daytime, this may be less of a problem because you have friends or family members who are available and by your side.
However, the nighttime could be trickier for monitoring: if everyone is asleep, this makes it harder for them to notice a seizure when one happens, even if you are in the same room.
Sometimes, you might wake up with a headache, or feel sore, and wonder whether you had a seizure the night before.
Or maybe your son or daughter has epilepsy. During the day, they are always with their teacher or other kids at school, so you may be less worried that they’d be alone if a seizure happens. However, as a parent during the night, you may worry about letting them sleep alone. Many of you have told us that you sleep in the same room, out of fear that a seizure will go missed.
Surely, in these situations, nights can be filled with fear, worry, and doubt. That’s exactly why we wanted to prepare this blog post for you, so you don’t stay in the dark. We are going to shine a light on:
- How common nocturnal seizures are
- Why they can be dangerous
- How you can know if you or your loved one had a nocturnal seizure
- How you can protect yourself by implementing a few, simple changes.
Let’s get started.
What are nocturnal seizures?
Any kind of seizure can be a nocturnal seizure, and they can happen to anyone who has epilepsy. Although, certain kinds of epilepsy are more prone to them: juvenile myoclonic epilepsy, awakening tonic-clonic (grand mal), Benign Rolandic, electrical status epilepticus of sleep, Landau-Kleffner syndrome, and frontal lobe epilepsy [1].
Some people have seizures that happen both during the day and at night [1], yet up to 45% of people have seizures predominantly during sleep [2]. If you only have nighttime seizures in your sleep, then you would have pure nocturnal epilepsy [1].
Although nocturnal seizures occur during sleep, some of their characteristics are similar to daytime seizures. During a nocturnal seizure, you may:
- cry out or make unusual noises, especially before muscles tense
- suddenly appear very rigid
- lose bladder control
- twitch or jerk
- bite your tongue
- fall out of bed
- wake up for no clear reason [3].
When do nocturnal seizures occur?
As the name suggests, they are seizures that happen during sleep, but this does not mean that they are limited to nighttime. They may also happen during a daytime nap [1].
According to Epilepsy Action Australia, there are more common times that you could have a nocturnal seizure: “Within the first or second hour after going off to sleep (early nocturnal seizures), one to two hours before the usual time of wakening (early morning seizures), within the first hour or so after awakening (early morning seizures)” [1].
Are nocturnal seizures dangerous?
Since nocturnal seizures mostly happen at night, they are less likely to be noticed, even by the person experiencing them [1]. Unfortunately, most cases of sudden unexpected death in epilepsy (SUDEP) occur after a seizure, and most deaths happen when people are in bed, supposedly sleeping [4].
However, if someone is there to provide first aid, keep the person on their side during a generalized seizure, or reposition them to keep their airway open, it may help limit SUDEP [5].
Another reason why nocturnal seizures may be dangerous is that people can get hurt: they may fall out of bed or have bruises when they wake up from injuries in the night. Since a lack of sleep can be a trigger for seizures in general, nocturnal seizures may also cause more daytime seizures [1]. Sleep monitoring solutions, like EpiMonitor, could help you understand when you've had a good night's sleep.
How can I know if I had a seizure in my sleep?
If there is no one there to witness a nocturnal seizure, it might be difficult to know whether you’ve had one. However, there are some signs to help you understand whether you or someone you love has had one:
- the bed is wet
- they’ve bitten their tongue
- they’ve fallen out of the bed
- they feel confused, exhausted, or sleep-deprived
- they have a headache
- they have bruises [3].
It can be challenging to separate a nocturnal seizure from sleepwalking or night terrors. As with other types of epilepsy, having a good history of seizures or an eyewitness account is important for the diagnosis [1]. Your doctor may do an EEG (electroencephalogram) to see the electrical activity in the brain. Sometimes, he may also do an MRI or CT scan. If someone only has nighttime seizures, a sleep study may be done to rule out other sleeping issues, like sleep apnea [6].
How can I prevent injury from seizures during sleep?
The correct treatment can help someone lower or prevent seizures. A doctor will decide on treatment based on the seizure type, the cause, and individual patient characteristics. Some treatment options include anti-seizure medications, the ketogenic diet, avoiding known seizure triggers, a vagus nerve stimulator, surgery, amongst others [6].
However, those with nocturnal seizures can take some preventative measures to reduce injury:
- choose a low bed frame
- put the mattress on the floor
- put a safety mat, like those for gymnastics, on the floor beside the bed
- mount lamps to the wall instead of keeping them on the nightstand
- move furniture away from the bed
- use a nighttime seizure monitor [3] like EpiMonitor for those in the US that alerts someone when the person has a possible tonic-clonic seizure.
It is important to recognize that there are no devices that have been proven to prevent SUDEP [7], but seizure alerting devices could help someone get seizure first aid more quickly [8].
EpiMonitor may be able to help.
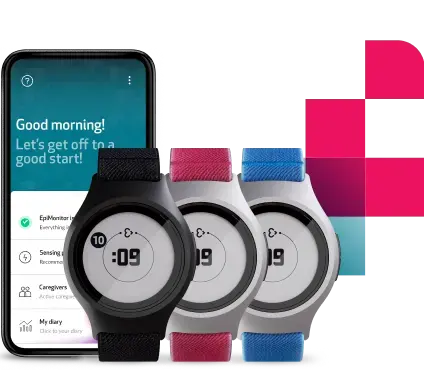
If you are looking for a solution like this, EpiMonitor may be able to help. EpiMonitor is our next generation wearable and smartphone app cleared by the FDA to detect possible generalized tonic-clonic seizures with 98% accuracy [9], both day and night. When it detects a possible tonic-clonic seizure, it sends a text message and makes a phone call to caregivers to alert them that you need help. It doesn’t matter how far you are from each other; you could be sleeping in adjoining rooms or different cities. The text message also contains your GPS location, in case your caregiver has to find you or send your position to emergency services.
In periods of rest, the false alarm rate (FAR) is low for both children and adults. In rest mode, 0.94 FAR per day for adults with high sensitivity, and 0.27 FAR per day for adults with low sensitivity [10].
This way, you can sleep more soundly, knowing that your loved one will be alerted and can come to help you quickly. Or, if you are a parent, with EpiMonitor, you can sleep in your own bed, with the peace of mind that you’ll be called if a possible seizure is detected.
What else does EpiMonitor have to help with nocturnal seizures?
EpiMonitor is your complete companion for epilepsy monitoring, keeping track of all your activity for you.
EpiMonitor is the only FDA-cleared wrist-worn wearable for epilepsy monitoring in the US. It’s currently available in the US, designed for adults and children 6 and up.
With EpiMonitor’s seizure diary you can keep track of your seizures, with the option to add self-reported seizures.
If you experience different kinds of seizures, such as focal or absent seizures, you can manually log these in your diary to ensure you and your doctor have a complete view of your seizure history.
Plus, you can easily review and add more information about your logged seizures in your personalized diary, including potential triggers and tracking your mood.
Everytime EpiMonitor detects a possible convulsive seizure, these alerts are stored in a “pending bar”. The pending bar shows you how many detected seizures you have to review before they show up in your seizure diary.
When reviewing a seizure, you can indicate if it was a false alarm, indicate how long it lasted, and add notes about how you were feeling beforehand. If you see a pending review for a seizure that you do not remember, it could possibly mean that you had a nighttime seizure.
You can review your physical activity and sleep alongside your seizures in your dairy, helping you to understand your lifestyle patterns and identify potential triggers.
This information can be used during conversations with your doctor, and you can easily download your report into a PDF to share with them via email.
We hope that this blog post has given you helpful and useful information on nocturnal seizures. By knowing more about them, you can be better prepared on how to protect yourselves and your loved ones. If you have any questions, feel free to email our support team at support@empatica.com.
References:
- https://www.epilepsy.org.au/about-epilepsy/understanding-epilepsy/nocturnal-seizures-seizures-during-sleep
- Malow, B. (2005). Sleep and Epilepsy. Neurologic Clinics, 23(4), 1127-1147. doi: 10.1016/j.ncl.2005.07.002
- https://www.medicalnewstoday.com/articles/326864#in-children
- Mostacci, B., Bisulli, F., Vignatelli, L., Licchetta, L., Di Vito, L., & Rinaldi, C. et al. (2015). Incidence of sudden unexpected death in nocturnal frontal lobe epilepsy: a cohort study. Sleep Medicine, 16(2), 232-236. doi: 10.1016/j.sleep.2014.09.019
- https://www.epilepsy.com/learn/early-death-and-sudep/sudep/sudep-faq
- https://www.cedars-sinai.edu/Patients/Health-Conditions/Nocturnal-Seizures.aspx
- https://www.epilepsy.com/learn/early-death-and-sudep/sudep/role-seizure-alerts
- Devinsky, O., Hesdorffer, D., Thurman, D., Lhatoo, S., & Richerson, G. (2016). Sudden unexpected death in epilepsy: epidemiology, mechanisms, and prevention. The Lancet Neurology, 15(10), 1075-1088. doi: 10.1016/s1474-4422(16)30158-2
- https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm?ID=K232915
- https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm?ID=K232915
We do not guarantee that EpiMonitor will detect every single seizure and deliver alerts accordingly. It is not meant to substitute your current seizure monitoring practices, but rather to serve as a supplement in expediting first-response time.