Is pulse rate the same as heart rate?
Background
The heart is essentially an electromechanical pump: a precise pattern of electrical instructions produces a corresponding pattern of mechanical contractions that circulate blood around the body through the blood vessels.
Using the appropriate sensors, we can measure either the electrical activity of the heart, the mechanical activity of the heart, or the circulation of blood in the blood vessels. Classic examples of each of these cardiovascular sensing modalities are:
- Electrical cardiac activity: electrocardiogram (ECG).
- A person’s heartbeat is triggered by electrical impulses, which are generated by the SA node (sinoatrial node), a small mass of specialized tissue located in the right upper chamber (atria) of the heart. The electrical activity of the heart spreads through the walls of the atria and causes them to contract, forcing blood into the ventricles. Each contraction of the ventricles represents one heartbeat.
- The electrical activity of the heart describes the controlled spread of electrical depolarization through the heart mass from one cardiomyocyte (heart cell) to its neighbors, as well as via a specialized electrical conduction system.
- Mechanical cardiac activity: ultrasound echocardiography (e.g. Doppler imaging).
- The mechanical activity of the heart is a synchronized muscular contraction that is produced as a result of the heart’s electrical activity. This contraction of the ventricles forces open and shut specific heart valves, thereby allowing the pumping of blood towards the periphery.
- Mechanical circulatory activity: photoplethysmogram (PPG).
- The mechanical circulatory activity describes the flow of blood (typically in the peripheral blood vessels) due to the muscular contraction of the heart. Metrics of mechanical cardiac activity such as stroke volume or contractility are also reflected by the circulation of the blood in the peripheries.
Although these three measuring modalities are deeply interrelated, it is important to highlight that they represent different but connected physiological phenomena, and that they can therefore be influenced by different factors. Hence, depending on what sensor we use and where we place it, we will obtain different information on cardiac activity.
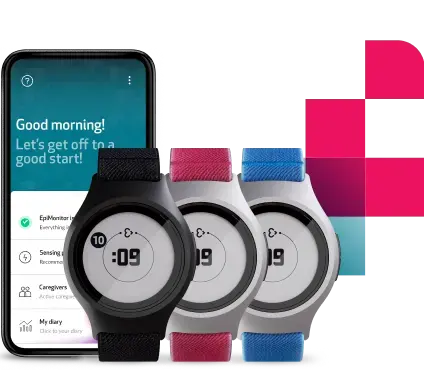
In recent years, wearable biometric sensors like the EmbracePlus have become commonplace for non-invasive medical research. Thus, in order to be precise, it has become necessary to clarify and distinguish between certain terminologies.
One such important distinction is between heart rate and pulse rate. Both of these measure the rate of cardiac cycles (usually in beats per minute) and they are sometimes used interchangeably. Though both heart rate and pulse rate are measures of cardiac activity, it is important to note that pulse rate can contain more “layers” of physiological and extraphysiological information/modulation.
How is Heart Rate measured?
Heart rate (HR) is a measure traditionally computed from the ECG, and thus is derived from electrical cardiac activity. The ECG signal is recorded by placing electrodes in contact with the skin - usually on the chest but also sometimes on the wrists. This ECG represents electrical cardiac activity. The electrical activation of the heart's main pumps - the ventricles - is reflected in an ECG signal via the 'QRS complex'. The dominant peak of this QRS complex is known as the 'R wave'. Heart rate is typically calculated by considering the average time between adjacent R wave peaks (referred to as the RR interval). This rate can be changed or modulated by the central (autonomic) nervous system in response to various internal stimuli (e.g. respiration, CO2 levels in blood, etc.) and external stimuli (e.g. stress).
A healthy ECG signal.
Is Pulse Rate the same as Heart Rate?
The same internal and external phenomena that modulate heart rate will also modulate pulse rate (since pulse rate depends on heart rate). However, any other physiological phenomena affecting the time delay between the R-peak of the ECG until the blood is transmitted through the circulation towards the PPG sensor (where it is reflected as a pulse in the PPG signal), will further modulate the measured pulse rate such that it will differ from the heart rate, though only to a minor extent. Often, however, researchers will use the term HR when in fact they are measuring the rate of cardiac activity by monitoring mechanical circulatory activity using the PPG. Although (as described below) both terms reflect the rate of cardiac activity, they should be using the term PR to more accurately reflect the technology used to compute this rate, as well as the possible physiological and extra-physiological factors that may influence it.
Various physiological factors may modulate this time delay, known as the pulse transit time, at different stages of the cardiovascular tree.
Firstly, the electromechanical coupling of the heart itself (i.e. how efficiently the electrical activity of the heart translates to mechanical contraction), then, the transmission of the mechanical activity of the contracting heart to accelerate the blood and the propagation of this impulse down the complex piping of the cardiovascular tree. Finally, there is the change in perfusion of the most peripheral tissues following the pulse that causes a change in the extent of circulation in these tissues, and therefore the amount of light reflected to the PPG sensor.
Each of these transmission steps has its own characteristics that may be influenced by physiological factors (e.g. blood pressure, blood vessel stiffness, etc.) and extra-physiological factors (e.g. stress, ambient temperature, and posture). These will act to modulate the pulse transit time, and therefore measured IBI, and make it differ from the original RR interval. [1] [2]
How a PPG sensor works to measure cardiac activity
PPG sensors measure blood circulation, which depends on the heart’s pumping quality, and therefore reflects the mechanical activity of the heart. Usually, the PPG sensors are placed at peripheral sites such as the finger, the wrist, or even the ear, and therefore they usually measure peripheral mechanical activity of the heart.
The PPG is an optical technique that measures the perfusion (or how much blood is circulating) through the blood vessels in the tissue under the sensor. Light from an LED is shined onto tissue, usually somewhere where it is comfortable to wear the sensor non-obtrusively, like the wrist. The sensor itself is typically a diode which translates the detected light intensity into the PPG signal: a series of pulses reflecting the pulsatile flow of blood.
Since the PPG is a measure of blood circulation (which depends on the heart’s pumping quality), it reflects the mechanical activity of the heart rather than the electrical activity of the heart. Hence, it is not precise to refer to time periods between cardiac cycles in the PPG as the RR-interval (since the R peak is an electrical phenomenon present in the ECG). Similarly, it isn’t precise to refer to the rate of cardiac intervals derived from the PPG as heart rate – since it is a peripheral and mechanical signal of cardiac activity. Instead, terms such as the inter-beat-interval (IBI) and pulse rate are more accurate.
Comparison of the ECG and PPG waveforms and intervals.
HR - Measuring cardiac activity using EmbracePlus
So what about the EmbracePlus? EmbracePlus uses a total of 9 LEDs and 4 photodiodes to record the PPG at the wrist. Hence, it records a peripheral and mechanical signal of cardiac activity, and it is more precise to refer to its measure of cardiac activity rate as pulse rate rather than heart rate. All wrist-worn biometric devices that use the PPG really are measuring pulse rate rather than heart rate, and FDA-cleared devices that use a similar technology usually refer to ‘pulse rate’ measurements. Although some smartwatch systems do allow for the recording of the ECG and therefore the heart rate, for that to work the user must physically touch and hold a specific part of the smartwatch acting as an isolated electrode, with their non-watch-wearing hand. Hence such systems cannot record the ECG (and they therefore it cannot calculate heart rate) in a continuous and passive way (i.e. without active user intervention).
HRV - PRV in EmbracePlus
What is Heart Rate Variability?
Heart rate variability (HRV) is a measure of the changes in the time intervals between adjacent cardiac cycles as measured by considering these RR intervals. A healthy heart is not a metronome; even under stationary conditions, the heart rate will be constantly changing. These variations are complex and non-linear, and are needed by the cardiovascular system to adapt to a changing environment in a quick and flexible way.
A multitude of factors can influence HRV, namely: the autonomic nervous system activity, blood pressure, respiration rate and emotional state. Quantifying HRV can therefore provide valuable scientific insights on these factors, particularly in response to a studied variable (e.g. a drug, a therapy, or a physical circumstance).
How HRV is measured
There are many metrics used to estimate the HRV. These can be derived from RR interval series spanning from just a few minutes (usually at least 5) to the whole day. HRV metrics are usually divided between time domain, frequency domain, and non-linear metrics. One of the most popular (time-domain) HRV metrics is RMSSD, i.e. the root mean square of successive differences in RR intervals (measured in ms). [3]
As seen previously, in the case of peripherally detected cardiac cycles like in the PPG, the time interval between adjacent cardiac cycles is more precisely defined as inter-beat intervals (IBIs).
From an IBI series, one can derive surrogate metrics of HRV: pulse rate variability (PRV) metrics. This tendency has been encouraged by the growing popularity of wrist-worn biometric sensors incorporating the PPG, since they can acquire signals for up to a number of days and with minimal discomfort to the user. Although HRV is the major determinant of PRV, a number of publications [4] in recent years have highlighted that it is not the only determinant. The same physiological distinctions between heart rate and pulse rate apply here for HRV and PRV.
Pulse Rate Variability as a reliable biomarker
Even though PRV can be influenced by factors not affecting HRV, even the same factors influencing both HRV and PRV may affect these in different ways and to different extents.[5] Even when the PR and HR are exactly the same, their amount of variation is not guaranteed to be the same. For instance, pace-maker-implanted patients whose heart is artificially paced at a constant rate (and therefore who do not demonstrate HRV), still show PRV. [3]
This difference is caused by the very origin of PRV: between the electrical activity that generates R peaks in the ECG and the peak on the PPG waveform used to identify the cardiac cycle, there are a number of variables that may modulate this time delay. These were already discussed previously when contrasting heart rate and pulse rate.
In conclusion, a growing number of authors [4] reckon that is more precise to consider PRV as a separate but closely related biomarker than HRV. PRV contains the same information as HRV, as well as several more layers of information from other physiological sources, which should not be considered as errors when comparing to HRV.
Do wrist-worn devices measure HRV or PRV?
As with heart rate and pulse rate, the same rationale applies for heart rate variability (HRV): wrist-worn devices using PPG technology (like the EmbracePlus) are actually measuring pulse rate variability (PRV). Although wrist-worn devices implementing ECG technology could, in theory, be able to measure HRV, the time spans generally required to get some reliable HRV metrics (at least 5 minutes) is too long for the user to comply without significant obtrusion/discomfort.
Nonetheless, research has shown that PPG methods have proven to yield discrepancies of less than 6% for most HRV measures [6], suggesting that wearable devices measuring PRV through a PPG sensor can still provide an accurate representative view of HRV.
So why do many research papers still use the term 'HRV' when actually they are referring to 'PRV'?
Despite the slight and subtle (yet known) differences between PR and PRV, and HRV and PRV, many research papers still use the term ‘HRV’, even when using a signal of mechanical circulatory activity such as the PPG (and hence they should be using ‘PRV’).
Although both measures are closely interrelated, it is important to distinguish between these terms to reflect the nature of the technology (i.e. sensors and signals) used to compute these metrics of cardiac activity variation, as well as the possible different factors influencing these metrics.
In the past, in a research setting, the subtle distinctions between HR/PR and HRV/PRV might have been implicitly clear. However, as the technology has advanced and these types of wrist-worn biometric sensors have become more ubiquitous (particularly to the general public), the need to explicitly distinguish between these terms has grown. To this end, regulatory bodies of medical devices have begun enforcing the use of the correct terminology (i.e. the distinction between PR and HR, and PRV and HRV) in such devices when referring to the technology used to measure cardiac activity.
Glossary of terms
- ECG (electrocardiogram) - a signal of electrical cardiac activity.
- PPG (photoplethysmogram) - an optically-derived signal of peripheral mechanical cardiac activity.
- HR (heart rate) – a measure of the rate of cardiac cycles derived from a measure of electrical heart activity such as the ECG (usually through a consideration of the time interval between adjacent R peaks on the ECG).
- HRV (heart rate variability) - a measure of the variation of the heart rate.
- IBI (inter-beat interval) - a different measure of the time interval between adjacent cardiac cycles more commonly used with the PPG signal.
- PR (pulse rate) – a measure of the rate of cardiac cycles derived from a measure of peripheral mechanical heart activity such as the PPG.
- PRV: pulse rate variability - a measure of the variation of the pulse rate.
- Biometric sensor/device: a device capable of recording one or more physiological signals, and extracting useful biomarkers from them.
Sources
- Differences in pulse rate variability with measurement site
- Ambient temperature effect on pulse rate variability as an alternative to heart rate variability in young adult
- An Overview of Heart Rate Variability Metrics and Norms
- Pulse rate variability: a new biomarker, not a surrogate for heart rate variability
- How accurate is pulse rate variability as an estimate of heart rate variability? A review on studies comparing photoplethysmographic technology with an electrocardiogram
- Comparison of HRV parameters derived from photoplethysmography and electrocardiography signals
We do not guarantee that EpiMonitor will detect every single seizure and deliver alerts accordingly. It is not meant to substitute your current seizure monitoring practices, but rather to serve as a supplement in expediting first-response time.