Can a wearable help decide who needs intensive care and when?
We are very pleased to offer you this special blog post, guest-authored by Dr. Nima TaheriNejad - Assistant Professor at TU Wien (Technical University of Vienna), Institute of Computer Technology.
The COVID-19 pandemic has locked us all in, it has got our attention.
We open our windows to clap and encourage our healthcare personnel because now we collectively appreciate the importance and hardship of their work.
While we take refuge in the safety of our homes, healthcare personnel resiliently fight with the danger face-to-face.
They show up every day, knowing that they are one small mistake away from contracting this feared disease. They provide care to the COVID-19 patients knowing that they are extremely exposed.
As if that were not bad enough, most healthcare facilities are understaffed, at least for coping with such a pandemic, if not always. The personnel is all exhausted for the extra hours of hard work and all they can hope for is that their exhaustion does not contribute to a moment of absentmindedness and that little but fatal mistake.
A question that I have been asking myself, and I think now all of us should ask ourselves more seriously, is: How can we reduce their burden?
Another characteristic of this pandemic is the recommendations of self-isolation, especially if you are certain that you have contracted it. That is, naturally, until the point that your symptoms are not too grave for home-care and you are not in the absolute necessity of professional care at a healthcare facility. And we all know why that is so: other than trying to minimize the spread of the virus, the healthcare facilities are, in most cases, way over their nominal capacities. Hence, any bed saved for critically ill patients over those whose bodies cope better with the virus means a soul saved.
However, an important question here is:
How to recognize that point, upon which you are in critical conditions that require professional care and referring to healthcare facilities?
We all have heard a story or two about patients who reacted way too late and lost their lives, and many stories about patients who went to healthcare facilities too early and took precious time from the healthcare personnel.
As an engineer, I am not qualified to answer that question, and tell you where that critical “point” is. However, I can give you a pointer to what hospitals have been using since the ’90s to decide which patient may need to be transferred to the intensive care unit (ICU).
Studies in the ’90s showed that certain biological measures are good indicators of potentially life-threatening health deteriorations.
They realized that by assigning a score to out-of-range values of these metrics and summing them up, the majority of cases, where patients were sent to ICU or lost their lives, could be predicted up to one day in advance. This led to various, slightly different, scoring systems, called Early Warning Score (or EWS) [14], which have been in use since then to enable an agile preventive measure against such severe health deteriorations.
To this end, a healthcare professional - usually nurses, go to hospitalized patients on regular intervals to manually measure the following metrics: heart rate, respiratory rate, systolic blood pressure, core body temperature, oxygen saturation level, and level of consciousness.
The higher your EWS, the more at risk you are, and sooner you should be subject to more intensive care.
The method, however, is not optimal for different reasons:
- It requires a lot of time and energy from the healthcare personnel, which is in great shortage these days.
- It exposes the highly on-demand healthcare personnel to a high risk since they have to come in contact with COVID-19 patients, or anybody else with highly contagious diseases.
- The EWS measurements are not captured continuously, which means some precious hours may be lost between every two checkups. Trying to reduce the health risk for the patients by more frequent checkups means a larger burden on the time and energy of healthcare personnel and higher exposure to risk.
- The procedure is not and often cannot be done at home by the patients themselves, which would be ideal for those in self-isolation due to COVID-19, or who were recently released from hospitals, due to the pandemic or otherwise.
The solution is trying to assess EWS automatically and using wearable devices - a topic that I have been working on during the past years.
Using wearables to assess EWS has its challenges too.
- One of the most important challenges is the reliability of measurements. While nobody wants a missed alarm, too many false alarms also have unwanted repercussions: the cost imposed on the healthcare system to have a closer look at the health status of the patients and the potential drop in sensitivity and reaction to the raised alarms are two of these repercussions. Causing unnecessary extra stress and psychological burden for patients and their families is another. However, these procedures are highly error-prone due to the uncontrolled conditions of use, and many non-idealities such as noise and movement artifacts. Along with a team of researchers from Austria, Finland, and the United States, we have been working on the identification [1,2] of such problems and addressing them [3-7].
- Another challenge is the number of sensors and devices required to measure all these parameters. Currently, the state-of-the-art in research is using a portable device and four or five sensory devices [3]. Even though the portable device can be a regular cellphone, as you can imagine, wearing so many sensors - especially continuously and for a longer time - is not very comfortable.
Some of these devices, such as the ones for blood pressure measurement, even in their digital form, are not made for continuous measurements. Some others, such as the ones used for direct respiratory rate measurements are extremely cumbersome to wear for a long time and may interrupt some daily activities since they involve a mouthpiece or a nosepiece.
There have been several efforts in trying to measure respiratory rate indirectly [8-13], but often leading to a very large measurement error (in the range of actual respiration rate at rest).
These challenges, sent us (me and a few of my students) to a mission, on which we had Empatica E4 wristbands as our companion. The E4 wristband already measures heart rate through photoplethysmogram (PPG) signals, which measure blood-volume pressure (BVP). We know that respiration affects BVP, an effect that can be used to indirectly extract respiratory rate. If we could do this, with small-enough errors, not only we could rid the patients from the cumbersome task of wearing a mouthpiece or a nosepiece, but also we could reduce the number of necessary sensors required for EWS assessment.
In a recent paper of ours [4], which was presented in February 2020 in Costa Rica during the Latin American Symposium on Circuits and Systems (LASCAS 2020), we showed our success in reaching our goal.
In “Reliable Respiratory Rate Extraction using PPG”, we proposed a frequency analysis technique that outperformed existing methods. More importantly, it managed to reduce the average error - despite movement artifacts - to a mere 3 breaths per minute, which is an acceptable error margin for the EWS assessment.
The importance of this work, and taking one step towards a more practical, automatic wearable EWS assessment system, is better understood in such times of hardship and overload for healthcare personnel.
Being able to measure respiratory rate using a wristband, which our experiments with Empatica showed to be possible, allows the development of applications to detect irregularities and disruptions of the respiratory system.
The early detection of a crucial symptom by using a consumer wearable could save the lives of many affected by COVID-19, without requiring expensive and hard-to-use medical devices.
We are committed to continue doing our very best to make this feat feasible.
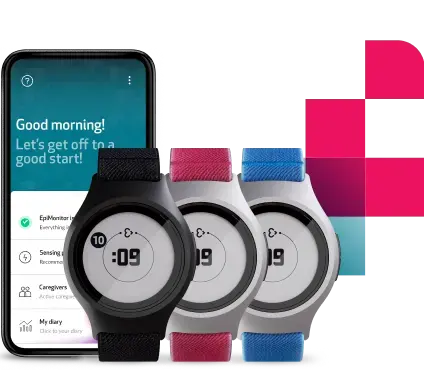
You can learn more about the E4 wristband by visiting our website or getting in touch with our team here. Empatica has recently launched Empatica Care, a powerful, AI-driven remote health monitoring platform that uses the EmbracePlus and bespoke software solutions.
References
- D. Pollreisz and N. Taherinejad, “Detection and removal of motion artifacts in PPG signals”, ACM/Springer Mobile Networks and Applications, pp. 1-11, 2019.
- N. TaheriNejad. “Wearable medical devices: Challenges and self-aware solutions”, IEEE Life Sciences, pp. 5–6, 2019
- M. Götzinger, A. Anzanpour, I. Azimi, N. Taherinejad, A. Jantsch, A. Rahmani, and P. Liljeberg, “Confidence-enhanced early warning score system based on fuzzy logic”, ACM/Springer Mobile Networks and Applications, pp. 1-18, 2019.
- D. Pollreisz and N. Taherinejad, “Reliable Respiratory Rate Extraction using PPG”, accepted for publication at 11th IEEE Latin American Symposium on Circuits and Systems – LASCAS 2020, pp. 1-4, 2020.
- M. Götzinger, A. Anzanpour, I. Azimi, N. Taherinejad, A. M. Rahmani, “Enhancing the Self-Aware Early Warning Score System through Fuzzified Data Reliability Assessment”, 7th EAI International Conference on Wireless Mobile Communication and Healthcare (MobiHealth), pp. 3-11, 2017. BEST PAPER
- A. Anzanpour, I. Azimi, M. Götzinger, A. M. Rahmani, N. Taheinejad, P. Liljeberg, A. Jantsch, N. Dutt, “Self-Awareness in Remote Health Monitoring Systems using Wearable Electronics”, Design, Automation and Test in Europe (DATE), pp. 1056-1061, 2017.
- M. Götzinger, N. Taherinejad, A. Rahmani, P. Liljeberg, A. Jantsch, H. Tenhunen, “Enhancing the Early Warning Score System Using Data Confidence”, 6th EAI International Conference on Wireless Mobile Communication and Healthcare (MobiHealth), pp. 91-99, 2016.
- P. Charltonet al. Extraction of respiratory signals from the electrocardiogram and photoplethysmogram: Technical and physiological determinants. Physiological Measurement, 38(5):669–690, 3 2017.
- R. A. Cernatet al. Real-time extraction of the respiratory rate from photoplethysmographic signals using wearable devices. European Conference on Ambient Intelligence, 2014.
- C. C. Mayer. Pulse contour analysis model for non-invasive determination of hemodynamical parameters. Phd Thesis, TU Wien, 2007.
- A. Schaefer and K. W. Kratky. Estimation of breathing rate from respiratory sinus arrhythmia: Comparison of various methods. Annals of Biomedical Engineering, 36, 03 2008.
- S. A. Shah. Vital sign monitoring and data fusion for paediatric triage. Phd Thesis, Oxford University, UK., 2012.
- J. Lazaroet al. Deriving respiration from photoplethysmographic pulse width. Medical and Biological Engineering and Computing, vol. 51:pp.233–242, 02 2013
- Morgan RJM, Williams F, Wright MM. An early warning scoring system for detecting developing critical illness. Clin Intensive Care 1997; 8:100.