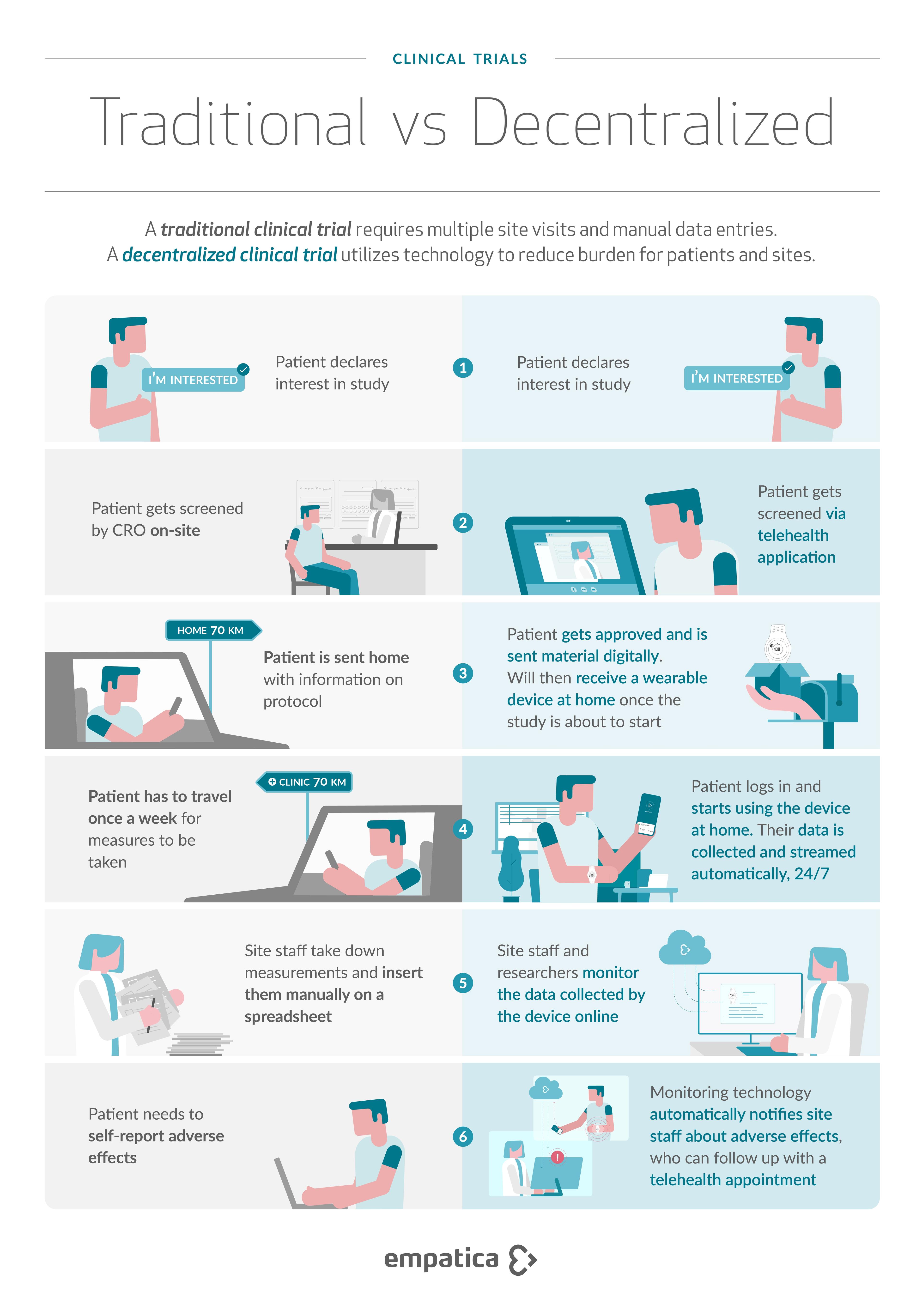
Decentralized vs Traditional trials: Differences and benefits
See the difference between decentralized, traditional, and virtual trials, and understand how sites and patients can benefit.

Clinical trials are a key driver of innovation in the life sciences field, ensuring the validation and subsequent delivery of novel drugs and treatments. Thus, it is imperative to seek means that would enable and help ensure trials run smoothly for years to come.
Enter decentralized trials, a novel way to conduct research that utilizes wearable sensors, remote patient monitoring, and digital endpoints, to enable the continuous and contact-free collection of data from participants, while limiting in-person contact.
Up until 2021, the fastest form of decentralization was digital data collection, with 296 trials using digital data collected that year. In comparison, the average from 2010 to 2016 was just 20 per year [1].
While we have witnessed a boom in home healthcare, understanding the difference between the different clinical trial models can help you evaluate which approach better suits your research.

Defining traditional, decentralized, and virtual trials
Traditional Clinical Trial
In traditional clinical research, data collection happens ‘on-site’. A site refers to where drugs and therapies are tested on humans, and can be a hospital or a clinic. The data is collected from these sites using available equipment, and entered into a database via an intermediary (a member of the study team or a healthcare professional).
Virtual Trial
A virtual trial is entirely site-less and fully remote, meaning no or extremely limited physical contact between clinicians and patients. Enrollment happens at a distance, and all data is collected remotely and autonomously, either through manual patient entry, or through portable sensors. This model is highly patient-centric, and done entirely through remote monitoring.
Decentralized Trial
A study that moves some or all of the trial participant interventions and prospective data collection outside of the traditional clinical trial sites and into the real world. These studies may use electronic platforms and data sources, mobile technologies, or ship investigational products directly to patients. Decentralized trials do not have to be 100% virtual. They offer the added flexibility needed to enable higher patient inclusion, balancing patient engagement with data integrity.
Decentralized trials may also be described as ‘hybrid’ trials, with some physical sites and some remote locations. These types of trials can maximize patient-centricity by allowing the study participant more flexibility in how she or he participates in the research.
Benefits of decentralized trials
A report by the Tufts Center for the Study of Drug Development (CSDD)[2] revealed that Phase 3 protocols collect an average of 3.6 million data points, a threefold increase in just under a decade. This increase, paired with a rise in eligibility criteria and strict timelines, means additional burden not just for patients, but also for site staff who are tasked with recruitment, participant retention, and data collection and input.
Meanwhile, in a study that looked at the engagement of patients in decentralized trials against traditional ones, the participant retention rate was 89% for the decentralized arm and only 60% for the traditional arm [3]. Remembering scheduled visits, taking time away from their family and work to attend them, and having to visit sites that can be hours away from their homes often make participating in clinical studies a challenge.
With decentralized trials, the participant burdens associated with traditional trials are reduced. This helps improve recruitment, retention, and allows sites to broaden trials to participants outside of local areas, in turn creating an opportunity to increase trial diversity.
The benefits of decentralized trials also include reduced workloads for site staff, with previously on-site data collection now taking place remotely, helping to reduce costs and increasing trial efficiency.
The Center for Information and Study on Clinical Research Participation’s (CISCRP’s) 2021 Perceptions and Insights Study [4] found that 85% of patients would be comfortable using a wearable device for clinical research. Moreover, 74% would be willing to collect all health data for a clinical trial at home on their own using technology, and only talking to the study team via video conference.
Closing remarks
While there are a variety of clinical trial models available depending on the needs of your trial, if conducted using the right tools, hybrid models can enhance participant engagement and subsequently data collection, while making it easier and more efficient for sites to manage the trial, in turn helping to reduce costs.
Technology plays a vital role in facilitating the real-world data collection needed for decentralized trials.
If you are looking to incorporate digital health technologies (DHTs) into your next hybrid trial, discover our Empatica Health Monitoring Platform or speak to our team to see how we can support your remote health monitoring and data collection needs.