4 things you need to know about sleep
“A well-spent day brings happy sleep,” said Leonardo da Vinci [1].
After a long day, you deserve a good night’s rest. You may even look forward to laying your head on the pillow. But, what if you have trouble falling asleep or staying asleep? If you have trouble sleeping, you aren’t alone because sleep problems affect the health and quality of life for up to 45% of the world’s population [2]. That’s a lot of people!
If so many of us have sleep problems, what are the side effects of a lack of sleep? What can you do to sleep better at night? We’ll discuss the answers to these questions in this blog post.
1. A lack of sleep or untreated sleep disorders can have negative side effects
Not sleeping enough can cause many physical and mental problems, among which:
- Untreated sleep apnea doubles the risk of heart arrhythmias.
- In children, sleep disorders cause school and behavior problems.
- Lack of sleep increases the risk of obesity and diabetes.
- Driving while drowsy causes 412 billion in productivity and property loss a year [3]. Also, not sleeping enough can cause
- high blood pressure
- depression
- substance abuse
- more doctor visits and hospital admissions
- and on-the-job injuries [4].
Thinking about the above information, it is easy to see why sleeping is important for your health. This is especially true for people with epilepsy.
2. Sleep is especially important for those with epilepsy
Sleep and epilepsy are closely related. Seizures are influenced by sleep and not getting enough of it [5]. For many people, a seizure trigger is a lack of sleep or sleeping poorly. Some people have nocturnal seizures, which can cause serious injuries or cause more daytime seizures. Epilepsy can also make sleep disorders worse, and make you feel worse during the day. Sometimes, seizure medicines can affect sleep by causing more drowsiness or problems falling or staying asleep [6].
So, what can you do to sleep better at night?
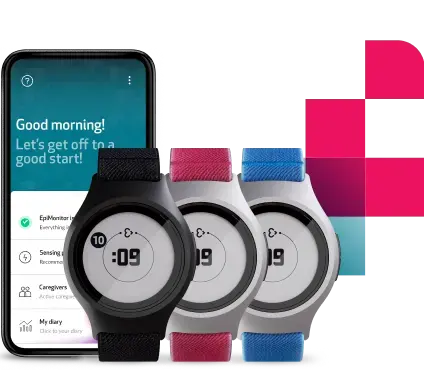
If you need help tracking your sleep, the Mate App shows you a complete sleep analysis.
3. There are ways to sleep better at night
There are many things that you can try to sleep better at night, and most of them are natural. Let’s see what the Epilepsy Foundation suggests.
- Decide on a fixed bedtime and wake time [6]. To get into a routine, you could set a reminder on your cellphone.
- Try to relax before going to bed to shut down and de-stress [6]. One idea is to write down a “to-do” list for the next day to help organize your thoughts and avoid distractions. Or you could listen to the radio or read a book to distract your mind [7].
- Turn off your phone and other electronics one hour before bed and remove them from the bedroom.
- Try to get some sun during the day to encourage your body to make melatonin (a hormone that regulates your sleep and wake cycles).
- Keep your bedroom dark, quiet, and cool (between 60-67 degrees F).
- Use fans or humidifiers to make white noise and comfort you.
- Create a comfortable sleep space with a quality mattress and pillow.
- Exercise during the day [6]. You can use Mate to see how physical activity and rest patterns match up.
- Avoid large meals before bed.
- Avoid stimulants and alcohol at night, and avoid drinks and food that have caffeine in the late afternoon. You should also avoid nicotine and alcohol close to bedtime.
- Before using sleep aids, speak to your doctor [6].
You can also keep a seizure and sleep diary [3], which can be helpful to identify lifestyle habits or activities that make you tired [7]. If you already use Embrace2, then we have an app to help you keep track of your seizures, rest, and physical activity information: Mate.
To keep track of your rest, Mate provides detailed statistics such as the time you woke up and went to bed, the number of tosses and turns, and interruptions. For example, if you feel especially tired one morning, check your sleep analysis in Mate. Although you may have been in bed for 8 hours, your sleep may have been interrupted throughout the night, resulting in less efficient rest.
To help you keep track of your seizures, all confirmed, detected seizures from the Alert App are automatically reflected in Mate, and you can add other types of seizures that you experience, too. Lastly, for physical activity, Mate shows you your step count, distance covered, duration of each activity, and total time spent moving.
If your doctor asks you to keep a sleep diary, you could show him your information inside Mate. It could help him to understand your lifestyle patterns better.
4. If you still can’t sleep, your doctor may be able to help
If you have tried to improve your sleep habits but still struggle, then you should talk to your doctor. According to the Epilepsy Foundation:
- He may order a test to understand if you have a sleep disorder or may prescribe medicine or devices to help you improve your sleep.
- Tests may be done to see if you are having nocturnal seizures.
- Your doctor may adjust your seizure medicine; keep in mind that you should never do this by yourself. Changing your seizure medicine may cause more problems.
- Some changes in mood, like depression or anxiety, may cause sleep problems, so speaking to a mental health provider could be useful. If the problems continue, then medicine for mood may be needed [6].
As we’ve seen, a good night’s rest is important, but it can be hard to get. Even so, we encourage you to keep applying good sleep habits and to talk to your doctor or healthcare provider when you have sleep problems.
Sweet dreams from us here at Empatica.
Disclaimer: The Mate App is not intended to make any diagnostic or treatment recommendations based on sleep or activity tracking, but instead, it can give you insights on your overall rest and physical activity.
Words worth reading
Sources:
1. https://www.sensacalm.com/blogs/news/best-sleep-quotes
2. Wade AG, Zisapel N, Lemoine P. (2008). Prolonged-release melatonin for the treatment of insomnia: targeting quality of sleep and morning alertness. Ageing Health. 4 (1): 11-12
3. Foldvary-Schaefer, N & Grigg-Damberger, M. (2009). Sleep and Epilepsy. Seminars in neurology. 29. 419-28. 10.1055/s-0029-1237115.
4. Banks, S., & Dinges, D. F. (2007). Behavioral and physiological consequences of sleep restriction. Journal of clinical sleep medicine: JCSM: official publication of the American Academy of Sleep Medicine, 3 (5), 519–528.
5. Kotagal, P., & Yardi, N. (2008). The Relationship Between Sleep and Epilepsy. Seminars In Pediatric Neurology, 15(2), 42-49. doi: 10.1016/j.spen.2008.03.007
6. https://www.epilepsy.com/living-epilepsy/healthy-living/sleep-and-wellness
7. https://www.nhs.uk/live-well/sleep-and-tiredness/how-to-get-to-sleep/
We do not guarantee that EpiMonitor will detect every single seizure and deliver alerts accordingly. It is not meant to substitute your current seizure monitoring practices, but rather to serve as a supplement in expediting first-response time.