The clinical importance of Heart Rate Variability
Heart rate variability (HRV) refers to the changes in the time intervals between consecutive heartbeats called inter-beat intervals (IBIs).
These fluctuations in heart rate reflect a key element of our flexibility in coping with environmental and psychological challenges and result from complex, non-linear heart-brain interactions and autonomic nervous system dynamics [1].
In our human self-regulatory systems, healthy functioning and well-being are related to our flexibility, adaptability, or resilience. These aspects are reflected within HRV’s large dynamics and fast responses to external and internal stimuli. While too much instability is detrimental to efficient physiological functioning and energy utilization, too little variation (a reflection of reduced regulatory capacity) indicates depletion or pathology [2].
HRV has been shown to be useful in predicting morbidities from common mental (e.g., stress, depression, anxiety, PTSD) and physical disorders (e.g., inflammation, chronic pain, diabetes, concussion, asthma, insomnia, fatigue) known to be accompanied by autonomic nervous system dysregulation [3].
In a recent study, involving young and healthy adults, inflammatory parameters were strongly associated with decreased HRV, suggesting an important interaction between inflammatory pathways and the autonomic nervous system [4].
HRV as an index of severe infection
The clinical importance of HRV became appreciated in the late 1980s when it was confirmed that HRV was a strong and independent predictor of mortality after an acute heart attack [5].
Since then, with the availability of digital, high-frequency, multichannel electrocardiogram (ECG) recorders, HRV has been widely studied, showing the potential to provide additional valuable insight into physiological and pathological conditions [6].
For example, HRV has been shown to decrease prior to the onset of severe infection and sepsis, thus providing a potential new biomarker to help in detecting both infection and sepsis [7].
Sepsis is the most common cause of mortality among critically ill patients and has been named as the most expensive in-patient cost in American hospitals, with an average annual cost amounting to $27 billion each year in the U.S [8-9].
Also known as blood poisoning, sepsis occurs when the body’s response to an infection causes damage to healthy tissues and organs. It can be caused by any type of infection, including the novel coronavirus (COVID-19). In recent clinical practice, it’s been noticed that many severe or critically ill COVID-19 patients developed typical clinical manifestations of sepsis.
Among the studies that investigated the relevance of HRV to monitoring the development of sepsis, the highest level of evidence was produced by studying the infant population [10]. Moorman, Griffin, and colleagues developed a new and proprietary measure, heart rate characteristics (HRC), to assess HRV in infants at risk of developing sepsis. They ran a large multi-center randomized controlled clinical trial involving over 3,000 neonates with very low birth weight. The study showed that displaying the HRC values at the bedside led to a reduction from 10.2 % to 8.1% in the in-hospital mortality rate: this reduction was statistically significant and clinically relevant.
How is HRV measured?
Currently, the primary method of deriving the HRV signal is to acquire the electrocardiogram (ECG) signal, apply appropriate QRS detection algorithms to locate the R wave and its peak, compute the RR intervals (refer to image), from which HRV indexes are derived. This process could sometimes result in errors in the HRV signal due to drift, electromagnetic and biologic interference, and the complex morphology of the ECG signal. A recent study has demonstrated the potential of the photoplethysmographic (PPG) signal to eliminate some of the problems with the ECG signal to derive the HRV signal [11]. In another study, electrocardiogram and PPG methods have proven to yield discrepancies of less than 6% for most HRV measures [12].
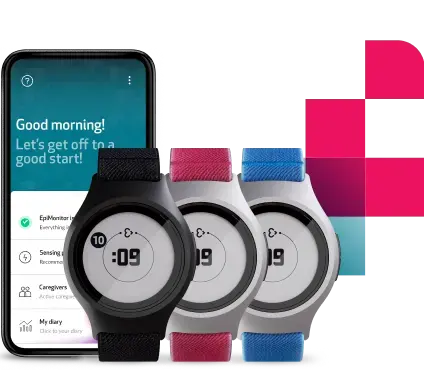
Among the wearable devices equipped with PPG sensors, research-grade devices such as the E4 wristband are the only wearables able to provide users with raw data that can be used to visualize PPG waveforms, verify the quality of the signal with each beat, and calculate an accurate estimate of HRV.
How to optimize HRV data
Given the proven benefit of early diagnosis in sepsis, there is an additional imperative to adopt means for diagnosing infection earlier, with the potential to save lives. In the midst of the current pandemic, the imperative of enabling early intervention has become even more urgent, together with the need for triaging effectively, reducing ER visits by high-risk individuals, lowering hospital readmission, and keeping healthcare workers safe.
The modulations of heart periods are naturally not the only manifestation of the autonomic regulatory mechanisms. Utilizing HRV data in combination with other primary vital signs (i.e. peripheral temperature, respiratory rate, electrodermal activity) as well as with machine learning (ML) techniques, can lead to more accurate diagnostic capabilities, helping to detect infection and identify the need for lifesaving interventions in a more timely manner. Multi-signal monitoring can also support more HRV studies in achieving a deeper understanding of physiological phenomena, the actions of medications, and disease mechanisms.
Vital signs monitoring platforms, such as Empatica Care, promise to achieve these very objectives, enhancing efficiency in both clinical and research practices, and leading to better medical outcomes.
If you are interested in joining the growing numbers of clinicians and researchers adopting Empatica Care for the remote health monitoring of your patients, research subjects, workforce, or local community, contact our team here or send any questions directly to care@empatica.com. You can also visit Empatica.com/care to learn more.
Sources:
- https://onlinelibrary.wiley.com/doi/abs/10.1111/psyp.12027
- https://www.frontiersin.org/articles/10.3389/fpsyg.2014.01040/full#B118
- https://www.aapb-biofeedback.com/doi/10.5298/1081-5937-45.1.03
- https://pubmed.ncbi.nlm.nih.gov/27534940/
- https://pubmed.ncbi.nlm.nih.gov/3812275/
- https://www.ahajournals.org/doi/full/10.1161/01.cir.93.5.1043#R6
- https://link.springer.com/article/10.1007/s11908-012-0282-4
- https://www.hcup-us.ahrq.gov/reports/statbriefs/sb204-Most-Expensive-Hospital-Conditions.pdfhttps://ieeexplore.ieee.org/document/1561529
- https://www.hcup-us.ahrq.gov/reports/statbriefs/sb168-Hospital-Costs-United-States-2011.jsp
- https://www.internationaljournalofcardiology.com/article/S0167-5273(12)00326-9/fulltext
- https://pubmed.ncbi.nlm.nih.gov/17946618/
- https://pubmed.ncbi.nlm.nih.gov/26737647/
We do not guarantee that EpiMonitor will detect every single seizure and deliver alerts accordingly. It is not meant to substitute your current seizure monitoring practices, but rather to serve as a supplement in expediting first-response time.