3 methods to reduce clinical trial costs with a DCT system
It’s a known fact - the costs of conducting clinical trials are very high. In a 2016 study, it was estimated that the average pre-approval costs per new compound were $2.6 billion. The estimate increases to $2.9 billion post-approval [1]. Researchers have argued that these “rising clinical costs have made the industry as a whole more risk-averse and less willing to take chances on novel medicines.” [2]
Not only are clinical trials costly, but their completion times are also long. According to DiMasi et. al, mean phase lengths are 21.6 months (1.8 years) for Phase 1, 25.7 months (2.1 years) for Phase 2, and 30.5 months (2.5 years) for Phase 3. The period between completion of Phase 3 and drug approval typically lasts one to two years, including six to 10 months for the New Drug Application (NDA) review itself, or even more if the drug is not approved after the first review. In short, the estimated mean completion time from Phase 1 until the release of a drug can take up to 7.4 years.
Furthermore, a 2006 study showed that a drug’s cycle times in development and regulatory approval are increasing. This means that a new drug can take even longer to go to market.[3] In addition to longer labor and running costs, DiMasi et. al. estimated that “roughly half of the total cost of bringing a new drug to market was due to opportunity costs associated with foregone investments over the drug development period.”[1]
Numerous factors may affect clinical trial expenditures, but some of the primary drivers in costs include [4]:
- Clinical procedure costs (15%-22% of total)
- Administrative staff costs (11%-29% of total)
- Site monitoring costs (9%-14% of total)
- Site retention costs (9% - 16% of total)
- Central laboratory costs (4% to 12% of total)
Fortunately, a wide array of tools and strategies are also available to help mitigate the barriers that researchers face. While there is no single solution, we hope we can provide you with information on the potential cost-cutting benefits of using Empatica’s Decentralized Trials Platform.
How can our decentralized trials platform help?
The adoption of mobile technology and implementation of digital procedures in trial protocols can help control trial costs across multiple processes, including site monitoring and retention, enrollment, and data collection. In fact, a cost analysis performed and published by the United States Department of Health and Human Services (HHS) reinforces these statements by suggesting several strategies that can alleviate trial expenditures, among which [5]:
- Wider use of mobile technologies, including electronic data capture (EDC)
- Simplified clinical trials protocols and reduced amendments
- Use of lower-cost facilities or at-home testings
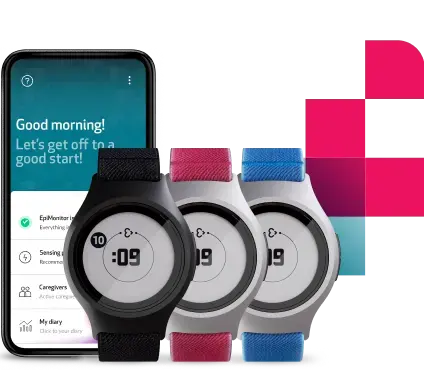
Empatica’s solution for decentralized clinical trials, comprised of medical-grade wearable EmbracePlus and remote monitoring platform Care, can be seamlessly integrated into trial models aiming to adopt the previously recommended strategies.
Mobile technology and electronic data capture (EDC)
The use of mobile technologies is one of the most effective and acknowledged approaches to reducing clinical trial costs. In their analysis, the HHS calculated that mobile technologies in trials can save about $0.4 million (up to eight percent of the cost per study) in Phase 1, ~$2.4 million (up to 12 percent of the cost per study) in Phase 2, ~$6.1 million (up to 12 percent of the cost per study) in Phase 3, and ~$6.7 million (up to 13 percent of the cost per study) in Phase 4.[5]
A key aspect of the use of mobile technology in clinical trials is the replacement of paper diaries with an Electronic Data Capture (EDC) system. Using EDC, researchers can collect and enter data into a data collection tool only once. With a paper system, on the other hand, data would have to be entered first into a case report form, then into an electronic system by a data entry group. Not only does this increases processing time, but transcription integrity is also affected.
The adoption of EDC has been examined in various publications with some profound results:
- 30% decline in study duration. [6]
- Saving throughout all the phases of clinical trials. Circa 5% in every phase, and 10% in phase 4. [5]
- The cost of a whole clinical trial can potentially be reduced up to 9.8%. [7]
EmbracePlus as an EDC system
Our EmbracePlus and Care platform allows subjects to use our mobile technology and the adoption of an effective EDC system. Some of the direct costs that can be saved include, but are not limited to [6]:
- Double data entry per page
- Data entry labor by a technician
- Data cleaning costs
- Printing and mailing each page
- Storing and archiving paper
- Fewer queries and faster resolution
The system streamlines the collection and transmission of clinical trial data directly from the trial participant to the researcher. EmbracePlus guarantees clinical quality data, subject use of the Care App automates the data flow, and the Care portal allows real-time data monitoring and exporting.
Based on the current literature, we inferred the cost-saving factors of EmbracePlus as an EDC system. A possible estimation of how much a pharmaceutical company can save per patient are the following:
- Phase 1: $367 per patient
- Phase 2: $2900 per patient
- Phase 3: $4860 per patient
- Phase 4: $702 per patient
Simplified clinical trial protocols
According to a recent study conducted by Tufts CSDD, “22.3 % of all procedures are considered to be non-core and can be considered “extraneous”[8]. Based on this information, the clinical procedure total (per patient) was also reduced by 22.3 percent in all phases.
These extraneous costs are associated with the collection of unnecessary data and the implementation of avoidable protocol amendments. Getz estimated that “approximately 15 to 30 percent of all clinical data collected is never used in NDA submissions, costing an additional $20 to $35 million in direct drug development costs for the average drug” [9]. By consistently collecting more pertinent data through wearable technology, the budget can be focused on what matters.
Empatica Care to simplify trial protocols
Aside from facilitating easy data collection, EmbracePlus and the Care platform can ease certain procedures to avoid extraneous and additional work:
- Availability to pre-enroll subjects remotely and prior to any site visits may help shorten study timelines.
- The Care portal allows researchers to reduce the hassle of complex setup by doing many steps virtually.
- There is no need for technical experts every step of the way. Data entry labor and data cleaning costs can be reduced since the patient data is collected automatically and available to download online.
In addition to these benefits for researchers, simplified clinical trial protocols may make it easier to recruit and retain patients by making trial participation less burdensome and exhausting. [5]
Use of lower-cost facilities or at-home testings
Costly infrastructure and overhead can be reduced by utilizing lower-cost facilities, such as local clinics and pharmacies, for data collection purposes. Local centers may also be used to conduct follow-up visits, minimizing travel and time costs for participants, and thereby possibly improving retention.
In their analysis, the HHS also reports how the use of lower-cost facilities and/or in-home testing can reduce per-trial costs by up to $0.8 million (up to 16% of the cost per study) in Phase 1, $4.3 million (up to 22% of the cost per study) in Phase 2, and $9.1 million (up to 17% of cost per study) in Phase 3, depending on therapeutic area. [5]
Running multi-site remote trials with EmbracePlus
As a web-based platform that shows real-time data feedback, the Care portal allows researchers not only to easily set up the study online but also to continuously monitor participants’ wearing time in a remote setting. Using our platform as a remote trial management system is cost-effective, reliable, and scalable.
- Minimizing site visits lead to fewer travel costs, fewer physician-administered procedures, and less physical data entry.
- Reduce the Hawthorne (observer expectancy) trial effect.
- Subjects wear a comfortable and minimal watch that is non-invasive and easy to use.
- All of this improves the overall experience for the patient, thereby improving patient retention and compliance.
Conclusion
There is no single strategy that can provide a solution to the increasing costs of clinical trials. Nevertheless, implementing technological and operational measures that can enable better and faster data collection, remote study management, and the simplification of otherwise complex processes, has great potential in the alleviation of clinical trial costs. Talk to our team to find out more about what EmbracePlus and the Care platform can do for you and your team.
Sources
- DiMasi, Joseph A., Henry G.Grabowski, and Ronald W.Hansen. Innovation in the pharmaceutical industry: New estimates of R&D costs. Journal of Health Economics (2016): 20-33.
- Roger Collier. Rapidly rising clinical trial costs worry researchers. 2009.
- Kenneth A. Getz. Hitching a ride with the speed demons of drug development. Appl Clin Trials (2006);15(12):22-24.
- Aylin Sertkaya, Wong, HH, Jessup, A, Beleche, T. Key cost drivers of pharmaceutical clinical trials in the United States. 2016.
- Examination of Clinical Trial Costs and Barriers for Drug Development, HHS. 2014.
- Neuer, Warnock, and Slezinger. The Upfront Cost Hurdle of EDC. Applied Clinical Trials. 1 April 2010.
- Eisenstein EL, Collins R, Cracknell BS, Podesta O, Reid ED, Sandercock P, Shakhov Y, Terrin ML, Sellers MA, Califf RM, Granger CB, and Diaz R. Sensible approaches for reducing clinical trial costs. 2008.
- Tufts CSDD. One in Five Procedures Generates Extraneous Clinical Trials Data. November/December 2012, Vol. 14 No. 6.
- Kenneth A. Getz. With clinical data, less is more. Applied Clinical Trials. 2010;19(1):28-30.
We do not guarantee that EpiMonitor will detect every single seizure and deliver alerts accordingly. It is not meant to substitute your current seizure monitoring practices, but rather to serve as a supplement in expediting first-response time.